NCDs
Non-communicable diseases (NCDs)
- Non-communicable diseases (NCDs) are diseases that cannot be spread from person to person via infection.
- They are sometimes referred to as ”chronic diseases” and often have a long duration.
- The four most common types of NCDs are cardiovascular diseases (like heart attacks and stroke), cancers, diabetes, and chronic respiratory diseases (such as chronic obstructive pulmonary disease and asthma).
- NCDs cause about 40 million deaths over the world each year
- NCDs can cause a range of health problems and are a major cause of disability. They can affect individuals in many different ways.


- The estimates of NCDs vary in different countries.
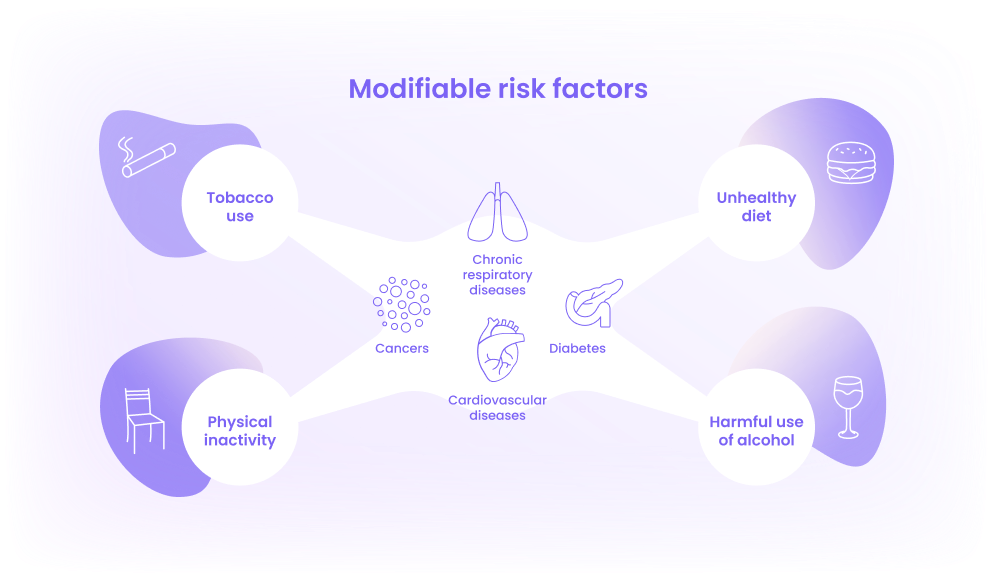
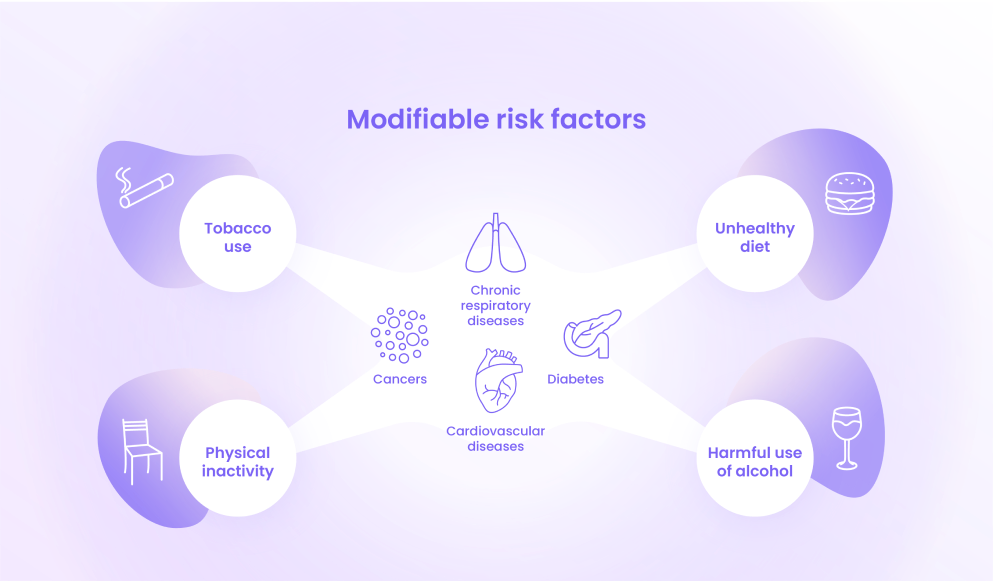
- The World Health Organization´s action plan focuses particularly on four types of NCDs — cardiovascular diseases, cancer, chronic respiratory diseases and diabetes.
- These are the most common NCDs and contribute to the most NCD-related deaths.
- They also share four behavioral risk factors — tobacco use, unhealthy diet, physical inactivity, and harmful use of alcohol
What are ”risk factors”?
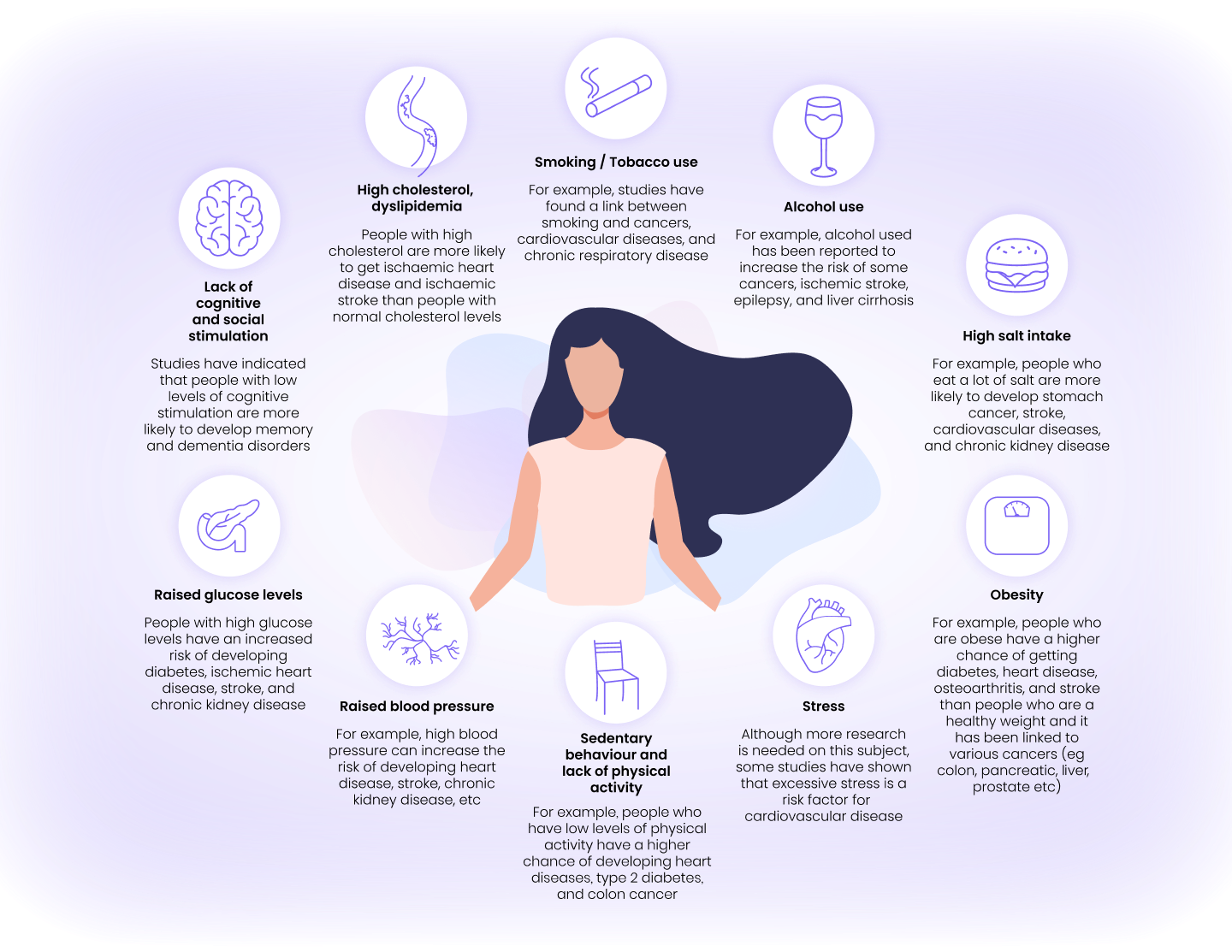
Research has shown that certain factors can increase a person’s risk of developing a disease. Risk factors refer to factors that increase a person’s chance of developing a disease. If you have a risk factor, your chance of getting a disease is higher than if you did not have that risk factor. For example, high salt intake is a risk factor for developing a stroke.
Risk factors do not always cause a disease, for example, you may know people who smoke but have never developed cancer. Also, just because you do not have a risk factor, it also does not mean that you will not develop a certain disease. This is because most diseases have multiple causes, some of which are not yet known, so it is impossible to predict them with 100% certainty.
Some risk factors cannot be modified, such as genetic or biological factors. For example, women have a higher risk of developing Alzheimer’s disease than men, but it is not possible to alter this risk. However, obesity has been shown to increase the risk developing Type 2 Diabetes. Weight can be modified, so this is a good example of a modifiable risk factor. Indeed, when overweight or obese people lose weight their risk of Type 2 diabetes reduces substantially.
Remember – just because you have a risk factor for a certain disease, it does not mean that you will necessarily develop that disease. It is also possible to develop NCDs even if you do not have any of the risk factors.
Protective factors
Some healthcare workers and researchers like to talk about “protective factors”. These are factors that can decrease your risk of developing a certain disease. These are usually the opposite to risk factors, for example exercise can protect against the development of diabetes (in this case exercise is the opposite of physical inactivity, which is a risk factor). However, protective factors are important because in some cases, risk factors are complex. For example, alcohol use can range from abstinence, mild to moderate drinking, heavy drinking, and excessive alcohol use or dependency. However, although heavy drinking is a risk factor for many NCDs, some studies suggest that light alcohol consumption is better than complete abstinence for some diseases, such as ischemic stroke.
Light or moderate alcohol consumption is therefore considered to be a “protective factor” for some diseases.
Examples of NCD risk factors
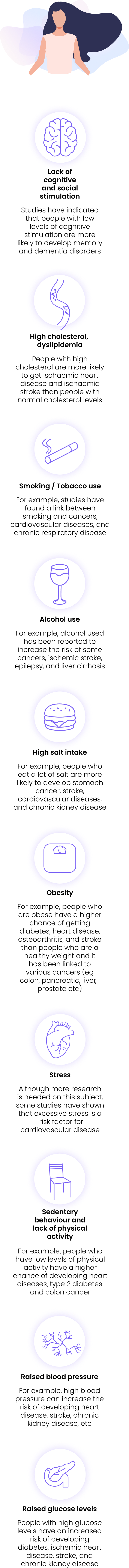
Modifiable
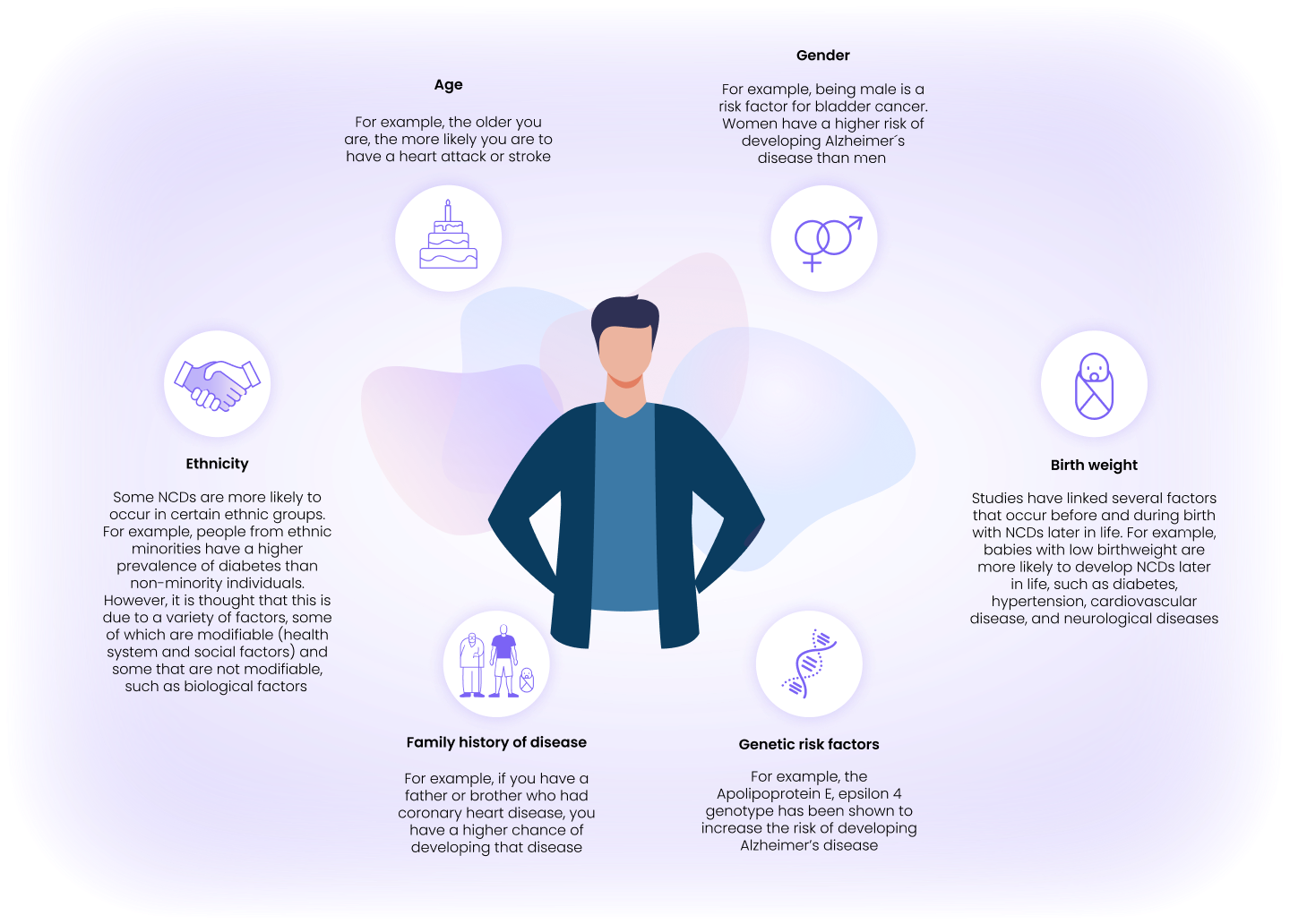
Non-modifiable
The importance of NCDs during the COVID-19 pandemic
NCDs have grown in importance during the COVID-19 pandemic for a number of reasons.
- People with pre-existing chronic diseases (especially older people) have an increased risk of being seriously ill if they get COVID-19. This risk is particularly relevant to older people who have multiple NCDs, which is often called “multimorbidity”. For example, studies from China and Italy report that COVID-19 patients who had multiple NCDs before infection have a worse prognosis, such as a higher risk of needing Intensive Care treatment as well as a higher risk of death.
- It might be more difficult to get a diagnosis of an NCD during the pandemic. Since the outbreak began, most countries have reduced non-urgent medical services. This was done to reduce the amount of face-to-face contact between healthcare providers and patients and sometimes because healthcare resources need to be allocated to the COVID-19 crisis. It can sometimes be difficult to see a physician face-to-face and waiting lists have often increased. This has led to delay in new diagnoses of NCDs. For example, a study in England reported a large decline in urgent referrals for early cancer diagnosis in the first wave of the pandemic.
- People who have pre-existing NCDs may experience disruption to their care and treatment. In a survey in the peak phase of the first wave (during April 2020) 56% of patients with cancer in the UK reported that the NHS had cancelled some of their treatment. Another study on English cancer patients showed that there was a decline in the number of attendances for chemotherapy treatment during the first wave of the pandemic.
- Some people have experienced difficulties getting access to medication and prescription services. This is sometimes due to drug shortages or in problems getting prescriptions from healthcare providers. In addition, some people worry about going into pharmacies to pick up medication in case there is a risk of contracting COVID-19. This is important because symptom control is vital for reducing negative outcomes in NCD patients. For example, if glucose levels are not well-controlled, people with diabetes can develop heart failure, myocardial infarction, and have a higher risk of death.
- Many risk factors for NCDs might increase during the pandemic due to lockdowns and social distancing. For example, it is important to maintain a healthy diet, exercise regularly, and avoid weight increase to reduce the risk of developing an NCD. However, the pandemic has changed the way that people can control such risk factors – for example, during lockdowns gyms and sports clubs sometimes close and as people are confined at home their physical activity levels often decrease. During the pandemic, many people have experienced stress, dietary changes, increased weight, lack of access to outdoor space, reduced exercise, and increased smoking and alcohol intake, which are all linked to developing certain NCDs.
- For people with already-existing NCDs, it is also important to control risk factors in order to manage their disease. For example, patients with Type 2 Diabetes need to have regular exercise, maintain a healthy weight, and control their blood glucose levels, as these can all increase the risk of negative outcomes (such as a higher risk of death, diabetic foot complications, hospitalization etc). Therefore, the management of NCDs, symptoms, and risk factors are all important during the pandemic.
- Interesting, many risk factors are interlinked and you can improve your health status by making some achievable changes to your lifestyle. For example, physical activity can reduce obesity while also reducing blood pressure and glucose levels. It also can reduce stress levels, improve depressive symptoms, and increase sleep quality. Therefore, even tackling one risk factor through prevention can have numerous health benefits.
- Prevention Trainer focuses on risk factors rather than specific diseases because many NCDs share common risk factors. Modifying your risk factors can help to reduce your risk of developing many different NCDs. Controlling and preventing NCDs can contribute to your overall wellbeing.


